Home Birth in Sheffield
This is my story, featuring birth photography taken by my partner in Sheffield. I never imagined myself having a home birth prior to COVID-19. I found comfort in the idea of a birth at a birth centre because should there be an emergency, I had better access to faster care. However, with the pandemic and increased restrictions from trusts across the country, I was afraid of the prospect of giving birth alone. I was afraid to be induced alone. I was afraid of my partner not being admitted while I was in labour, and most of all, I was afraid of being left alone postnatally. I had confidence in myself to be able to birth alone, but I could not imagine recovering from whatever type of birth I had postnatally by myself.
After many discussions with my midwife, she reassured me that a home birth could be the right choice for me if I wanted it. There were no restrictions on who could be present during a home birth during the pandemic. I knew my partner and I could be together the whole time, all going well. I decided to go for a home birth.
The Sweep and Fever
At 40+3 weeks pregnant, on Thursday, 11 March, I saw the midwife who offered me a sweep. I consented, she told me I was 1cm dilated, and she sent me on my merry way saying that if it is a successful sweep, things should start happening within the next 24-48 hours. After the sweep, I decided to go on a walk through the woods and when I returned home, I had a fever. I tried showering and waiting it out for a few hours before I decided to call triage. I was worried the sweep gave me an infection.
When I called triage, they immediately defaulted to COVID because of the fever, though I had no other symptoms. It’s kind of understandable that they would think this, but they refused to think it was anything else. After a couple of hours and being bounced between various people, I managed to convince triage to give me a lateral flow test to prove I was COVID negative and to then investigate what else might be causing the fever. No surprise, my COVID test came back negative. They hooked me up to various machines for monitoring and what they said “would only take about 30mins” took three hours…
Normally, I wouldn’t mind, but with COVID restrictions in place, I was completely alone in this room while my partner was left waiting outside in the car. The labour ward was very busy and the midwives only came in to check on me about every 30-40 minutes. I needed to pee. I was thirsty. I was hungry. I was hooked to these machines and couldn’t move. I was very uncomfortable. Eventually, when the midwife said “everything appears to be normal and okay with baby, but we’re just waiting on these blood results which will take anywhere between 1-6 hours to get back to us” I decided to self discharge against their advice. I was not going to wait that long alone in this room. I left and told them to call me with the results and pending the results, I would return if needed.
It was over 24 hours later when they finally called me with the blood results. The results showed that I did have an infection of some kind, but they were “not overly concerned” because it could just be cold symptoms. They asked if I had developed any other symptoms other than the fever (which at this point had completely disappeared). I told them that I had started to cough a bit more which was causing a headache. They repeated that they weren’t overly concerned, but if my conditioned worsened, to call them again.

A Botched Hospital Visit
I went to bed that night and awoke at 2:30am with a raging headache, a cough that wouldn’t stop, and intense pain in my abdominals from the pressure of coughing. I waited an hour to wait for the paracetamol to kick in and see if it would go away. It didn’t and so I called triage again. The midwife who answered reviewed my file, consulted with a doctor, and again repeated that they were “not overly concerned” but if I wanted to come in for extra pain relief or antibiotics, I could. They also wanted me to take another COVID test if I came in. They said all of this would take about 30 minutes…where had I heard that before?
I told them over the phone that I would only consent to enter the hospital if my partner could accompany me for support as I did not feel I could do this alone. They refused. After a lot of discussion on the phone, the midwife finally agreed that both M and I would receive a lateral flow test in the car. If it was negative, we could go in. We drove to the hospital. Upon arriving, a midwife came out to the car and told me I had to go into the hospital, alone, to have my observations taken first and then a COVID test. I refused saying they could give me the COVID test first in the car, as agreed, and then we could both go in. The midwife said “I’m not arguing” and walked away. We drove to A&E thinking we might as well try there as we’re already out. A&E also refused entry to M. We decided to leave and go home, but not before three doctors and consultants were chasing us through the parking lot urging us to come back inside. They still would not admit M, though, so we left.
Contractions Begin and Stop
By the time we got home it was 5am on Sunday morning. We went back to bed. I awoke at 7am with contractions.
So far, we had barely slept the past two days. We began tracking the contractions via an app and when the app said “go to the hospital” we called the midwife. The midwife arrived around 10am. She observed me for a little while and asked if I wanted a vaginal examination to see how far along I was. I consented. I was only 1cm. Cue crushing defeat. I knew that this could mean that I had anywhere between several hours, days, or weeks yet. The midwife left saying to call if anything changed.
My contractions died away completely by the afternoon. I took a nap as I hadn’t really slept the past two days. I awoke around 7pm, went downstairs, called some friends and bounced on my birth ball. Meanwhile, my partner went for a nap.




Active Labour Begins at Home
Around 9:30pm, I decided to go back to bed. Not even 30 minutes later and my contractions were back with a vengeance. They were incredibly intense and came in rapid succession.
I was screaming. Not necessarily due to pain, but I found the sound of my voice and screams comforting through the contractions. My partner slept through it. I finally decided I couldn’t do this alone anymore, I needed his support and I woke him up. He is a deep sleeper…
The midwife arrived around 11pm. By this point, I was hooked up to my TENS machine, which was helping me through the contractions. I was transferring constantly between the floor and our bed. I barely wanted to move. I was always on all fours. Between contractions, tried to rest. During contractions, I roared and moaned.
I heard the midwife talking to my partner and heard her say “I think she’s *only just* in active labour.” This statement would colour the rest of my birthing experience. I inwardly felt a bit of dread. If I was only just in active labour, then that meant I still had another 6cm to go. I imagined it would take many hours and that I needed to really pace myself and conserve as much energy as I could.


High Blood Pressure and Pre-eclampsia
Throughout the majority of my pregnancy, I had been under consultant led care. This was mostly due to a previous partial molar pregnancy and a family history of pre-eclampsia. By week 36, I was finally discharged from consultant led care as everything in my pregnancy had been completely average and low risk. They signed me off for a home birth.
Back to my labouring at home…the midwife was consistently monitoring my blood pressure every 30 minutes and baby’s heart beat every 15 minutes.
My first blood pressure reading was “quite high,” but it was only the first one and she wasn’t overly concerned at that point. “Not overly concerned” was a phrase I kept hearing a lot…
After a couple of blood pressure readings later, the midwife was beginning to get concerned. My blood pressure was high and continuing to rise. I had just got out of a hot shower, another way to cope with the contractions, and my partner had gone downstairs to fill the birth pool, when the midwife asked if I could pee in a jug so she could check for any protein in my urine.
It took me a while before I could manage it in between contractions and vomiting (the contractions were so intense by this point they were causing me to purge quite a bit). When the midwife tested my urine, there was protein present which was a cause for more concern for her. She called the hospital to get a second opinion on what to do, but it was sounding like she was wanting us to transfer.



The Transfer to Hospital
Because of my consistently high blood pressure (and gradually increasing blood pressure), the protein in my urine, and my family history of pre-eclampsia, both the hospital and home birth midwife wanted me to transfer in. However, I really appreciate my midwife as her stance was “It’s advised that you transfer in, and I would advise it as well, however it is completely your choice what you want to do. You can stay home or transfer. You get to decide.”
At this point, though, nothing, and I mean NOTHING the midwife said computed to me. I could not hear her or understand her. My partner acted as translator. He simply repeated verbatim what the midwife said and I could somehow listen to and hear him. I did not want to transfer in. I was scared of being left alone. I was scared of my partner being told to leave shortly after I gave birth. I had an overwhelming sense that I would be alone if I transferred. My partner did an incredible job advocating on my behalf whilst also being sensible when I could not be. We both recognised the risks associated with staying home, but rather than deciding definitively whether to transfer or stay right away, we compromised. We decided that we would wait 30 more minutes for the next blood pressure reading. If it had increased or remained high risk, then we would transfer. If it managed to decrease, we would stay.
My blood pressure had gone up again.
I resigned to a transfer and as silly as it sounds, felt crushed that I couldn’t go into my birth pool that was waiting for me downstairs as the ambulance had been called and was on its way.
My partner helped me to get dressed and downstairs to wait for the ambulance. What felt like a mere 10-15 minutes to me for the ambulance to arrive was in fact an hour and a half. In hindsight, I felt deprived of my birth pool which I could have been in during that time, but we couldn’t have known the ambulance would take that long.
Arrival at Hospital and the Second Stage
Before arriving at the hospital, and whilst waiting for the ambulance to arrive, my partner and I now recognise what must have been my transition phase at home. Between contractions, I was requesting a birth pool at the hospital and asking if I could have both an epidural and go into the pool. I was crying and saying “I can’t do this, I just want it to stop.” In my mind, I kept recalling the words the midwife had said earlier in the evening “she’s only *just* in active labour.” I felt I still had hours and hours to go. I would not be able to keep this up. However, I now believe this to have been my transition meaning I was very close to giving birth.
The ambulance arrived and it took a very long time to get me from the lounge to the ambulance. We were stopping every few seconds for my contractions.
In the ambulance, I was strapped onto a gurney whilst laying on my side. I appreciated that they were okay with me on my side and did not attempt to force me onto my back. Laying on my side was already incredibly uncomfortable. My partner was not allowed into the ambulance with me and instead followed behind in his car.
The journey in the ambulance was awful. Pot holes and road bumps made everything even more uncomfortable.
I then felt something change in my body. I felt an intense pressure on my pelvic floor during contractions. I told the midwife, “I think my body is pushing.” She asked me to try and breathe through the contractions and not to push. We were almost there.
Once at the hospital, I was wheeled into a room, still strapped to the gurney. I remember passing people in the reception of triage and screaming in their faces as I contracted. Part of me saw it as a kind of out-of-body experience. On one hand, I felt the present intense contractions and on the other, I was laughing at the picture of a highly pregnant person being wheeled into a hospital and screaming in the faces of other pregnant people. I kind of felt bad about the image I was showing them of what their future could be…
The Pool and Another Transfer
Immediately upon arriving in the birth room, I got off the gurney and leaned on the edge of the birth pool. I was dead set on getting myself into that birth pool even though it wasn’t even filled with water yet. The idea of being in water was honestly the only thing getting me through. With one foot on the step leading up to the pool, I paused for a contraction. I felt what I can only describe as a very large bubble descend upon my pelvic floor and get pushed out of my vagina during the contraction. I remember saying “what the fuck is this??” and then I felt a gush of fluid on my legs and my feet become drenched. I realised it was my waters breaking.
My partner just arrived into the birth room to the scene of me trying to get into the empty birth pool and the midwives telling me that I can’t because there were large amounts of meconium in my waters.
I didn’t care. I was getting in that damn pool.
The midwives insisted that I had to be transferred to labour ward to be seen by a doctor. They wanted me to get onto a wheelchair so they could transfer me across the hospital. At this point, remember, my body was beginning to push during every contraction since I arrived at the hospital from the ambulance. I told everyone that my body was pushing and there was no way in hell I was sitting on that wheelchair.
The midwives were adamant that I had to get on the wheelchair and be transferred. They also kept telling me not to push, to breathe through it as they didn’t know how far along I was and I could be pushing prematurely. I essentially screamed back at them saying “I hear you, I am not trying to push, but my body is doing it anyway!”
I was also still dead set on having my water birth and getting in the pool. I knew there was no pool on labour ward where doctors are involved. Now, my partner says he doesn’t recall a midwife ever saying this, but I remember hearing it. I admit that I could have imagined it given the state that I was in. The only way I made it onto that wheelchair was because I heard (whether real or not) that if I got into the wheelchair and got checked by doctors, then I could come back and get into the pool.
I was CLINGING to the idea of that pool.
Now, I want you to picture a cat being held over water. The way their back arches and their claws are out. That was me on that wheelchair. I did not want to sit down as my body was pushing. I hovered my body over the seat, arms shaking, fingers clawing into the arm rests yelling “I can hold it, just GO!” The midwives wouldn’t move until I sat down, which took a lot of convincing from my partner for me to do.


The Birth
As soon as I was wheeled into a room on labour ward, I toppled out of the wheelchair, onto the floor on all fours as people rushed to strap monitors onto me. I was completely unaware of them. I could only feel the intensity of the contractions and the overwhelming desire to push. I still had midwives telling me not to push and to just breathe.
A midwife suggested I might be more comfortable on the bed rather than the floor. She kept reiterating that I could stay on all fours, but perhaps on the bed where it would be softer on my knees. She lowered the bed as far down as it would go and…it was still too tall for me to climb onto. There was no stool or step for me to use to get onto the bed. My partner went to the other side of the bed and was heaving me up onto the bed.
I was still being told not to push. I kept repeating, I’m not…my body is.
Someone handed me gas and air and told me to breathe. I did and after a couple of puffs…relief. This was the first form of pain relief I had had since taking off my TENS machine several hours ago at home. I inhaled through the mouth piece and screamed as I exhaled. There was no peaceful “breathe baby down” in this story. I was roaring. Not exclusively because of the pain, but because the sound comforted me.
“I can see baby’s head,” a midwife said.
It was at this moment that I could feel myself tearing. I want to be clear that while it was painful, it lasted mere seconds before it was over and in no way negatively impacted my birth experience. The opposite actually happened, where I was curious and almost amazed that I was aware of the sensations of me tearing. I remember saying to my partner “I can feel myself tearing,” and him saying “there’s nothing we can do, just breathe.”
I remember thinking to myself, well maybe if someone just applied some lube it wouldn’t be so bad, but that thought disappeared quickly when the head emerged.
Two more pushes and S was born.



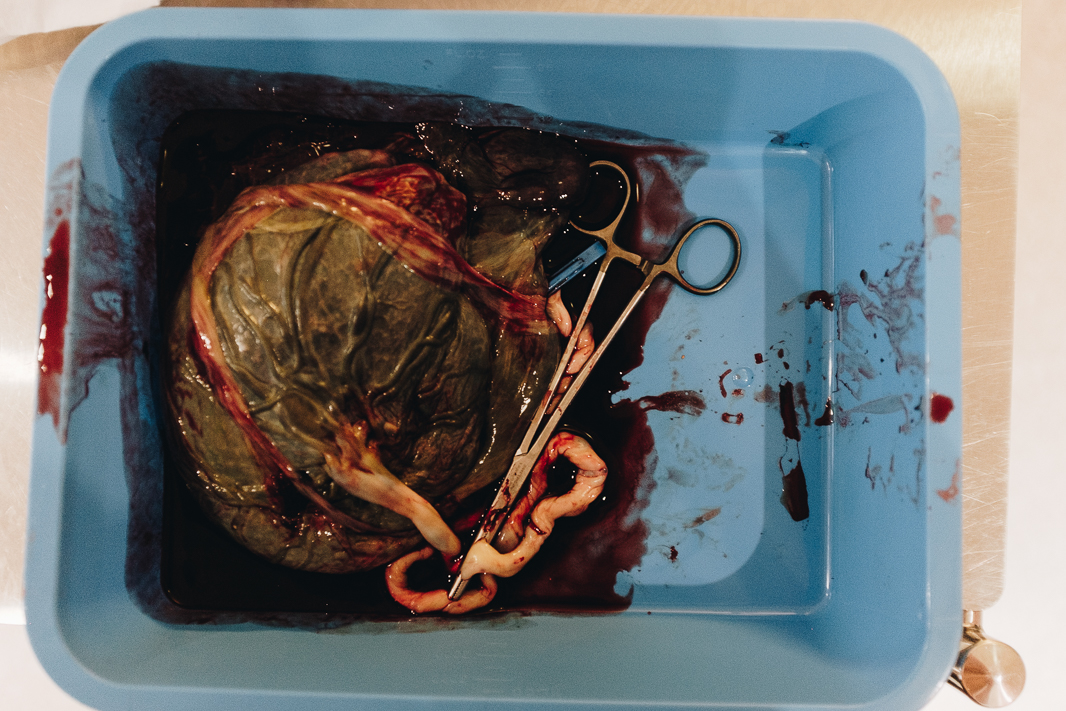
The Afterbirth
Following S’s birth, my partner was with us the entire time. She was never asked to leave, despite me hearing stories and the own trust’s website saying that partners would need to leave “shortly after the birth” typically 30 minutes to one hour after. My partner was with me for six hours after the birth on labour ward. This is honestly what made my entire birth experience so positive. Spending all of that time together as a brand new family of three was priceless.
For the birth of the placenta, I had wanted to have a physiological birth, but it wasn’t to be. After an hour of waiting for contractions to kick back up and the placenta to come, I received an injection in the thigh to encourage things along.
Even with the injection, I never felt any desire to push. My body was done. The midwife was absolutely brilliant, though, and rather than recommend I go to theatre, she suggested that she help to birth my placenta by gently pulling on the cord and palpating my stomach as I pushed when directed. She was very gentle and went incredibly slow through the whole process. Any time she met resistance while pulling the cord, she paused and waited. She was never forceful. Within minutes, my placenta was out.
The Tear
The part I dreaded the most finally arrived. I held my breath as the midwife examined me to see how bad my tear was. I knew I tore as I could feel it when it happened, but I didn’t know how much. After copious amounts of gas and air, the midwife couldn’t be sure if I had a second or third degree tear.
A second degree is one where the midwife can stitch me up whereas a third degree tear involves tearing of the anus which must be done in an operational theatre. A doctor was called in for a second opinion. It was confirmed to be a second degree tear (whew!).
As the midwife began administering the local anaesthetic, I was inhaling gas and air as if my life depended on it. I couldn’t feel what she was doing. There were times where I even asked my partner if S was okay and still on my chest as I couldn’t feel him. He was and he was fine. My whole body was numb and tingly. I told the midwife that this experience reminded me of college. But I quickly clarified that it was the gas and air that reminded me of college not having my vagina stitched up. Everyone else sucked a bunch of helium in college, right? No…just me then? Alright…
During most of this part, the midwife and I were simply having a casual conversation. I didn’t feel anything except the really odd sensation of thread moving through you but without feeling it really. It’s really hard to explain.
We talked about the cost of childbirth in the US vs the UK. I said how after every NHS visit people should be given a bill to show the cost of the care they received so that they better appreciate the NHS.
The worst part of being stitched up is when the midwife realised she missed a spot in the application of the local anaesthetic. She told me to take some really good, deep puffs because this was going to hurt. And holy shit, did it hurt. Now this scream was a proper scream of “I am in so much pain” unlike my earlier screams during contractions. I squeezed my partners hand so hard that he was also wincing in pain. This feeling was worse than feeling myself actually tear or giving birth or any of the other contractions.
The midwife apologised profusely and it was over very quickly.
Heading Home
After I was all stitched up, my partner held S for some skin-to-skin and they did all of the checks while I went for a shower. The midwife brought tea and biscuits into the room and we had a very nice, calm time for a couple of hours.
Due to some temperature problems, I ended up being transferred to the postnatal ward with S. M wasn’t allowed to attend on that ward, so she went home and cleaned up the house from all the home birth stuff. I didn’t mind being alone at this point as we had about 5-6 hours together on labour ward.
By the end of the day, after S’s temperature rose, we were discharged and went home.
We placed a sleeping S into his cot by our bed and crawled under the duvet of our bed. We shut our eyes to enjoy a well-deserved rest…the sounds of S crying reached us and our journey into parenthood began…


0 Comments
Trackbacks/Pingbacks